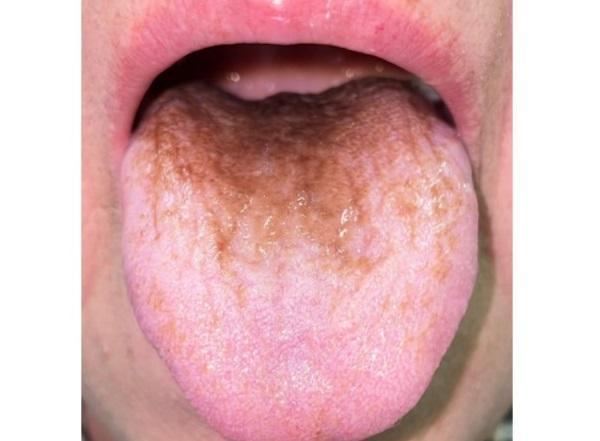
A 69-year-old woman developed black hairy tongue syndrome (BHT) after taking an antibiotic commonly prescribed to treat bacterial infections.
Certain types of antibiotics, including penicillin and cephalosporins, can cause this unusual benign condition characterized by the appearance of hypertrophic and elongated filiform papillae on the dorsal surface of the tongue. However, this incident is believed to be the first reported case of TNT specifically caused by moxifloxacin.
“Physicians should be aware of pathogens or lifestyles that can cause BHT, and it is important to counsel about the possibility of developing BHT before starting treatment to avoid patient anxiety or premature discontinuation of treatment,” write the authors, led by Dr. Mikiro Kato from the Department of Infectious Diseases, University of Tsukuba Hospital, Japan.
After the appearance of a brown spot on the tongue, the patient went to the clinic. The woman has a history of Sharp syndrome – mixed connective tissue disease (MCCT) – a rare connective tissue disease characterized by a combination of individual signs of lupus erythematosus, scleroderma, rheumatoid arthritis, polymyositis. For this reason, she took daily oral steroids. She also had high blood pressure, high cholesterol, diabetes, and osteoporosis.
Approximately three months before her visit to the clinic, the woman underwent reconstructive surgery due to tendovaginitis of the flexors of the index and middle fingers of her right hand. The procedure was complicated by osteomyelitis caused by Mycobacterium chelonae.
She was treated for six weeks with intravenous tobramycin and imipenem and oral clarithromycin. She was then switched to oral antibiotics (moxifloxacin and clarithromycin).
Within 10 days of switching to oral antibiotics, the woman noticed changes in the color of her tongue. When she went to the clinic, she did not have a fever or any other symptoms. She denied any change in medication, herbal medicine or Chinese medicine, and smoking and alcohol. In addition, the patient reported that she did not use any tongue scrapers, cleaners, or mouth rinses.
Further examination showed that her vital signs were normal. Examination of the oral cavity showed that the mucous membrane was dry, and on the back of the tongue became brown in color with elongated, filiform lingual papillae that looked like a carpet. However, the woman did not have cavities, bad breath, bleeding, discharge, or exudates.
Due to the absence of significant symptoms, a tongue swab was not taken. The doctor made a preliminary diagnosis: discoloration of the tongue due to nutrition or BHT, as a result of taking antibiotics. For two weeks, the woman was observed: daily oral hygiene and cleaning of the tongue by scraping was carried out. However, the appearance of the language has not changed.
The patient refused further antibiotics. Due to the lower sensitivity of moxifloxacin to isolated Mycobacterium chelonae, this antibiotic was discontinued and she continued to take clarithromycin only. Within two days after she stopped taking moxifloxacin, her tongue returned to normal.
