More than a hundred years ago, local anesthetics began to be used in dentistry in its various sections: from therapeutic dentistry to maxillofacial surgery. Since their early use, local anesthetics have continued to shape and advance the field of dentistry, providing a means by which a variety of procedures can be performed in outpatient and inpatient settings. In dentistry, local anesthetics have the added benefit of providing hemostasis to the surgical site, resulting in increased visualization and decreased blood loss. A variety of products are available on the Russian market. Although the mechanism of action of these local anesthetics is similar, each drug has its own unique characteristics, allowing the practitioner to tailor the choice of local anesthetic to the needs of the patient and the requirements of the procedure. The purpose of this article was to introduce the basic evolution of local anesthetics currently available on the market and their unique properties.

The fight against pain is one of the most important problems of modern medicine, which is enshrined in the patient’s rights to pain relief (Federal Law of November 21, 2011 No. 323-FZ “On the fundamentals of protecting the health of citizens in the Russian Federation,” paragraph 4 of Article 19) [1].
The effectiveness, safety and predictability of local anesthesia are a leading indicator of the quality of outpatient dental practice [2].
Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage. In 1979, this definition was adopted as the main one by the International Association for the Study of Pain [3], [8].
Pain has been a faithful companion of man and is the result of most dental procedures and diseases; therefore, good control of dental pain is inevitable and feasible. The administration of local anesthetics has become the standard of dental care. All local anesthetics are effective and have a high safety margin in all patients, including children. The choice of local anesthetic depends on the timing of the surgical procedure, the patient's medical history, and the interaction between local anesthetics and the patient's regular medications. The use of vasoconstrictors is a priority for surgical dental bleeding, but they should be used with caution in patients with cardiovascular disease to avoid dental complications [3],[4],[9],[10].
Dentists must be experts in dental anesthetic techniques and the pharmacology of local anesthetics as they are the most commonly used drugs in dentistry [3],[4].
The purpose of this article was to analyze the evolution of local anesthetics in dentistry.
Materials and methods of research
Analysis of information resources, publications, literature until August 2023:
- foreign sources ( Scopus, PubMed, MedLine, Google Scholar, etc.),
- domestic sources (eLibrary.Ru, CyberLeninka, etc.)
Results and discussions
History
The history of the dental specialty is closely related to medicine. Before the advent of local anesthetics, natural plants and preparations were first used to relieve toothache, and removal was carried out without anesthesia, and toothache was treated empirically with mallow poultices, a few glasses of wine or cognac, or herbal infusions. Such medicine developed from the times of Ancient Egypt and Greek culture until the nineteenth century, until the advent of injection syringes and opiates for dental pain. The first recorded dental anesthesia in history was performed in 1885 by alveolar inferior nerve anesthesia by surgeon William Stewart Halstead. The drug administered was a combination of cocaine and adrenaline. In 1905, 2% procaine with 1:50,000 epinephrine was introduced, giving rapid access to dentists throughout the world. Procaine, propoxycaine and tetracaine were the most commonly used local anesthetics until the mid-1940s [1-10].
Lidocaine was synthesized in Sweden in 1943 and introduced to the market in 1948, becoming the first local amide anesthetic to be used in clinical practice, replacing procaine. The latter was withdrawn from trade in many countries precisely because of its rapid absorption into the blood, where it could reach high levels [4], [5].
Articaine was synthesized in 1973 and introduced into the dental clinic in 1976 and approved in Canada in 1984 and in the United States until 2000. Articaine has the special characteristics of both aminoamide and aminoester anesthetics. Its popularity has grown rapidly and is now replacing the use of lidocaine in dental anesthesia. Articaine is the only starch with an additional ester group. Thus, the molecule undergoes double metabolism, partly in the liver and partly in the plasma. This characteristic gives it a high ability to diffuse into tissue. It is always sold together with a vasoconstrictor (adrenaline 1:100,000 or 1:200,000) [4],[5].[6].
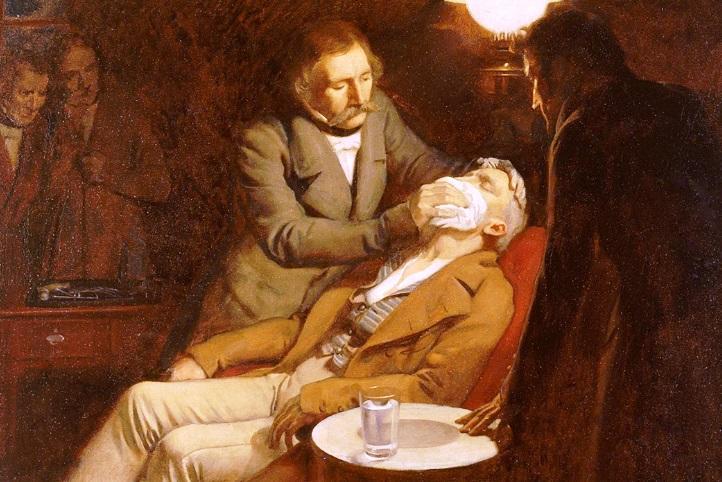
Figure No. 1. First use of ether in dental surgery, 1846. Oil painting by Ernest Borda. Source of information [11].
Local anesthetics in dentistry
Currently, local anesthesia in dentistry consists of blocking a small or large nerve ending through contact with an active substance. Local anesthetics can be divided into two main categories: esters and starches. The molecules commonly used in clinical practice today are all included in the second category: lidocaine, mepivacaine, articaine and bupivacaine. Although different techniques can be distinguished between periosteal anesthesia (infiltration) and nerve block itself, in addition to individual methods (intraligamentary, intrapulpal, etc.), the route of administration is always injection. For this reason, various molecules are sold in tube form. Each tube contains the active ingredient in a predetermined amount, possibly in combination with a vasoconstrictor in an aqueous solution [1-10].
Lidocaine has been the most commonly used drug in dentistry since its introduction in 1948 and is currently considered the gold standard for clinical use. It was a drug that replaced older anesthetics such as procaine (Novocaine). It has a rapid onset of 2 to 3 minutes with longer and deeper anesthesia. It is available in various concentrations; the most common are 1 and 2% cartridges with adrenaline 1:100,000 and 1:50,000.
Mepivacaine is an amide type of anesthetic, available only in cartridges formed with a concentration of 2 and 3%. Mepivacaine is combined with a vasoconstrictor at a 2% concentration. Ideal for patients with an absolute contraindication to taking vasoconstrictors.
Articaine has recently been introduced into dental practice. It is an amide type, but it has an ester group, making it a single drug hybrid, thus being metabolized in the plasma as well as in the liver, where most of the process occurs, resulting in an inactive metabolite called articainic acid. Its vasodilating effect is equivalent to lidocaine. It has a rapid clearance time of approximately 27 minutes compared to 40 minutes for amide anesthetics. It offers 90 minutes of pulpal anesthesia and 3 hours of soft tissue anesthesia, which is a smart choice for most dental procedures. It is available in dental cartridges at 4% concentration, with epinephrine at concentrations of 1:100,000 and 1:200,000 [4],[5].[6].
Figure No. 2. Conducting local anesthesia in modern dentistry. Source of information: photograph from the author’s personal practice.

Conclusion
Pain management remains one of the most pressing problems in dental practice.
For a long time, pain and dentistry have been associated with each other, but with the advent of new drugs, medical technologies, theoretical knowledge and the latest equipment, dental practice has become virtually painless.
List of used literature
1) Federal Law of November 21, 2011 No. 323-FZ “On the fundamentals of protecting the health of citizens in the Russian Federation”, paragraph 4 of Art. 19 . URL: https://minzdrav.gov.ru/documents/7025-federalnyy-zakon-323-fz-ot-21-noyabrya-2011-g (date of access: August 1, 2023)
2) Anesthesia in dentistry children and adults/S. A. Rabinovich, Yu. L. Vasiliev, L. A. Zavodilenko [and others]. — Moscow: GEOTAR-Media, 2022. — 336 p. : ill. — DOI: 10.33029/9704-6954-5-PRD-2022-1-336
3) Jänig W, Baron R. Complex regional pain syndrome is a disease of the central nervous system. Clin Auton Res. 2002;12(3):150-164. doi:10.1007/s10286-002-0022-1
4) Local Anesthetics in Odontology. Enrique Hernández-Cortez, Cecilia G. Sandoval Larios and Juan Carlos Flores-Carrillo. Published: July 22nd, 2020 DOI: 10.5772/intechopen.91738
5) Cervino, G. Milestones of Dentistry: Advent of Anesthetics in Oral Surgery. Dent. J. 2019, 7, 112. https://doi.org/10.3390/dj7040112
6) Options for drug provision for Russia. Lessons from European countries and the whole world – Vlasov V.V., Plavinsky S.L. Moscow, Media Sfera Publishing House, 2013 118 pp.
7) Gabunia N.Yu., Khaniev A.A., Matytsin N.O. , Dental surgical checklist as a tool to improve patient safety //Bulletin of Roszdravnadzor. – 2023. – No. 1.
8) Book: Peterson's Principles of Oral and Maxillofacial Surgery, Published: Springer Nature, 4th ed., 08 August 2022
9) Clinical recommendations (treatment protocols) for the diagnosis of complete absence of teeth (complete secondary adentia, tooth loss due to an accident, extraction or localized periodontitis). Approved by Resolution No. 15 of the Council of the Association of Public Associations “Dental Association of Russia” dated September 30, 2014, official website of the Dental Association of Russia URL: https://e-stomatology.ru/(date accessed August 1, 2023)
10) Maxillary -facial surgery: national guidelines. Author: Kulakov A.A. Publisher: GEOTAR-Media, 2019
