There are about 40 trillion people living in the world. microorganisms for which our body is also a home. If we express the number of microbes in kilograms, then 3.5-4 kg of microflora is inside us and travels with us.1

This entire microbial cosmos is actively involved in almost all physiological vital processes, break down sugars, fiber, proteins, fats, converting them into simpler compounds, produce individual proteins, vitamins (group B, vitamin K), regulate the absorption of calcium, iron, vitamin D.
Normally, in the oral cavity, lactobacilli prevent the growth and reproduction of staphylococci and streptococci – the causative agents of sore throat, pharyngitis and gum disease. And, also, lactobacilli take an active part in the formation of local immunity.
From the perspective of medical science, the role of normal microflora of the oral cavity is as follows:
- Development of local lymphoid tissue
- Suppression of the proliferation of pathogenic types of bacteria entering the oral cavity. Normal flora microbes suppress the reproduction of other species and genera of bacteria due to higher biological potential (high reproduction rate), competition for a food source, by changing the pH of the environment, the production of alcohols, hydrogen peroxide, lactic and fatty acids, etc.
- Synthesis by representatives of normal microflora of proteins such as lysozyme, acidophylline, bacteriocins, which have bactericidal activity against foreign microorganisms
- Increasing readiness for immune reactions (immune tone)
- Ensuring self-cleaning of the oral cavity
- Supplying the body with amino acids and vitamins that are secreted by the microbiome during metabolism
- Stimulating the secretion of salivary and mucous glands
With the use of antibiotics, poor oral hygiene, the development of destructive pathology of teeth and gums in the oral cavity, tumor processes, the composition of the microbiota changes.
An imbalance changes the immune status in the oral cavity, increasing the risk of stone formation and the appearance of sialoliths (salivary stones) in the ducts of the salivary glands.
What oral disease most often worries patients?
The condition of the dental system and gums has a huge impact on the quality of life. This is the calling card of every person. If oral hygiene is impaired and the biological balance is shifted, gingivitis can develop – inflammation of the gums. The accumulation of dental plaque and a decrease in the ability of the oral cavity to self-cleanse contribute to the appearance of gingivitis.
At the beginning of the disease with gingivitis, the dentoalveolar connection is not disrupted, but the mucous membrane is irritated and gum pockets are formed, due to an increase in the distance between the tooth and the soft tissues. Such pockets are an ideal environment for bacteria to multiply.
An imbalance of lactic acid and pathogenic flora, against the background of a decrease in the defenses of the oral cavity, especially due to allergies, fungal and viral infections, as well as uncontrolled use of antiseptics or antibiotics, is the most common cause of the development of gingivitis.
Background diseases and conditions in which the risk of gingivitis increases are hormonal disorders, diabetes mellitus, hypo- and avitaminosis, immunodeficiencies, pregnancy, blood diseases, and gum injury.
The most common complaint of patients with gingivitis is the appearance of a heavy and unpleasant odor from the mouth, which can hardly be masked by standard hygiene products – pastes, deodorants, rinses, chewing gums.
Subclinical manifestations of dysfunction in the oral cavity do not always require aggressive treatment tactics, and they can be corrected by bringing the state of the oral microbiota into a balanced state.
This is achieved by changing the diet and using dentabiotics, which include live strains of “beneficial” microflora, vitamins and prebiotic components.
Thus, in a randomized, double-blind, placebo-controlled clinical trial in 40 non-smoking patients aged 18 to 55 years with healthy gums or mild gingivitis, the ability of the probiotic strains L. plantarum KABP™ 051 and L. brevis KABP™ 052 to colonize oral tissue was confirmed and their preventive properties for gingivitis5
Lactobacillus brevis and Lactobacillus plantarum were initially found in the oral microbiota of all respondents (L. brevis found in higher abundance than L. plantarum), indicating that both bacterial species are commonly found in the oral cavity of healthy individuals. Over the course of six weeks of treatment, both types of bacteria increased significantly in the group of respondents receiving probiotic bacteria compared to placebo. At the end of the study, mean concentrations of L. brevis and L. plantarum were 10 times higher in the probiotic group than in the placebo group (Figure 1).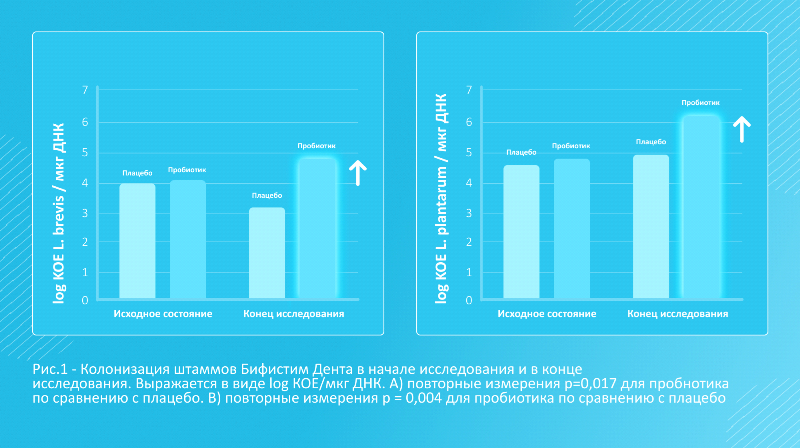
As expected, none of the study subjects had gingivitis or deep periodontal pockets at the end of the study.
With the advent of dentabiotic* BIFISTIM® Denta a completely unique and favorable situation is emerging for people at risk for developing gingivitis or already suffering from gingivitis.
BIFISTIM® Dentacontains two strains of probiotic bacteria Lactobacillus plantarum and Lactobacillus Brevis and vitamin coenzyme Q (ubiquinone),
Clinical studies have shown that Lactobacillus plantarum and Lactobacillus brevis support oral health5:
- L. plantarum and L. brevis are natural oral microbiota and are found in the saliva of healthy people4;
- They demonstrate high antagonistic activity against pathogenic and conditionally pathogenic microorganisms of the oral cavity (P. gingivalis, T. denticola and F. nucleatum)4;
- Have good adhesive abilities to oral tissues and maintain the effect throughout the day for a single use4;
- Resistant to volatile components of mouth rinses (thymol, menthol, myrtenol and other constantly changing conditions of the oral cavity (temperature of food, liquid, acidity)4
< p>There are practically no contraindications for BIFISTIM® Dent, with the exception of individual intolerance.
It is important that coenzyme Q10 (ubiquinone) helps to increase the protective properties of the oral mucosa and reduces the risk of re-infection.
Convenient use of a balanced dentabiotic* is the key to replenishing the population of beneficial microflora in the human body.
Microbial “landing” is able to preserve and maintain the normal state of the oral cavity, positively influencing the course of pathological processes, restoring a healthy smile, pleasant relationships and a comfortable state.
BIFISTIM® Denta is taken 1 tablet per day with meals. It is recommended to keep it in your mouth until completely dissolved. Duration of treatment – 1 month.
BIFISTIM® Denta – dentabiotic* for oral health!
Regular use has a cumulative effect.
Dietary supplement. IS NOT A MEDICINE
Certificate of state registration AM.01.07.01.003.R.000172.02.22 OT 02.18.2022
*Dentabiotic – probiotic complex for oral health.
Links:
- Kirill Stasevich. Microbes for health //Science and life. – 2018. – No. 9. – P. 70-75. Archived on October 11, 2018.
- Krendelev M.S. NORMAL MICROFLORA OF THE HUMAN ORAL CAVITY //Modern problems of science and education. – 2015. – No. 5
- Beaugerie L and Petit JC. 2004. Antibiotic-associated diarrhoea. Best Practice & Research Clinical Gastroenterology, Volume 18, Issue 2, Pages 337—352
- Bosch M., Nart J., Audivert S. et al. Isolation and characterization of probiotic strains for improving oral health. Arch Oral Biol. 2012 May;57(5):539-49.
- Nart J., Jiménez-Garrido S., Ramírez-Sebastià A. et al. Oral colonization by vilactobacillus brevis KABPTM-052 and Lactiplantibacillus plantarum KABPTM-051: A Randomized, Double-Blinded, Place bo-Controlled Trial (Pilot Study). J Clin Exp Dent.2021:13(5) e 433-9.
Advertising LLC Marketing Medical Digital, erid: 2Vtzqumpirk
