Microchips that mimic human body parts may seem futuristic, but these devices, called organs on chips, are already being used to study human biology. Made of plastic, with grooves lined with cells and channels through which air and fluids are transported, these chips can mimic aspects of organ structure and function.
The chips have been designed to mimic many different parts of the body, including the tissues of a beating heart, air-filtering lung cells and electrically active brain cells. This technology could help speed up drug discovery, enable personalized medicine, and even reduce the need for animal experimentation.
Researchers in projects supported by the US National Institute of Dental and Craniofacial Research (NIDCR) are taking advantage of this technology by placing parts of the human mouth on chips to find better ways to treat oral diseases. From tooth-on-a-chip research at Oregon Health and Science University (OHSU) to development of a salivary gland chip at the University of Rochester and more, scientists are testing dental materials, repurposing drugs to treat salivary gland dysfunction, and studying the inner workings of the oral cavity.
In the early stages of human disease research, scientists conduct research on animals or cells that are cultured in a petri dish. However, results from animals don't always transfer to humans, and cells can behave differently in the 2D bowl than they do in the human body. Organs on a chip, also known as tissue chips, occupy a unique space between living systems and cultured cells, providing an environment for 3D tissue growth and more realistic responses.
Luis Bertassoni (far right) and his team designed a miniature dental system to carefully observe the interaction between dental materials, the microbiome and tooth tissue.
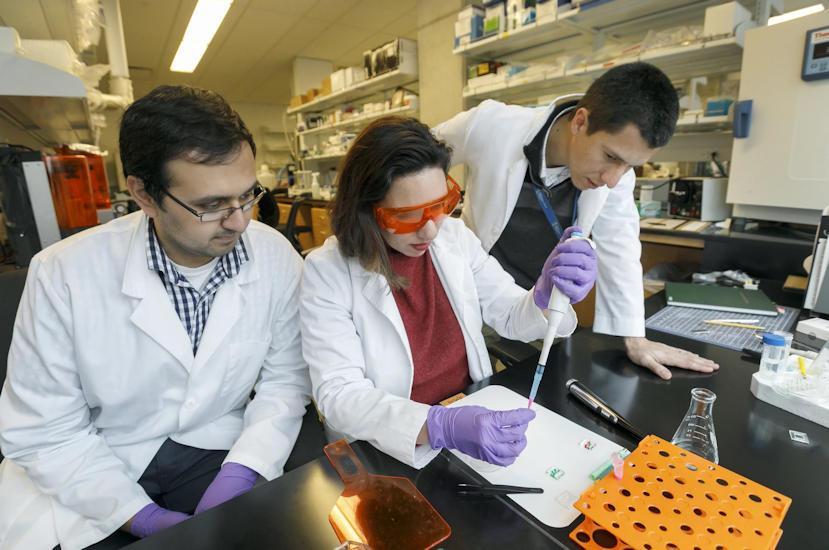
“In a sense, we put a window on the cloth and we can watch how it reacts,” says Dr. Luis Bertassoni of OHSU, Ph.D. A couple of years ago, Bertassoni's team developed the first tooth on a chip to understand how microbes and biomaterials like dental fillings interact with teeth.
The stamp-sized chip consists of a thin piece of a human molar sandwiched between two chambers. One chamber, representing the inside of the tooth, contains the dental pulp, which is made up of cells that keep the tooth alive; the other chamber mimics the outside of the tooth, where it comes into contact with oral bacteria and dental materials.
While scientists have carefully studied animal dental materials and cell culture, they have not fully understood how the cells inside a real human tooth react. Using their newly developed tooth on a chip, Bertassoni's team set out to fill this gap in a 2020 study. On the cut surface of the molar, the team applied an etchant, primer and adhesive, materials used for standard dental restorations such as cavities and chipped teeth.
Using a microscope to peer through the transparent rubber casing of the chip, the researchers observed how the pulp reacted in real time to materials deposited on the tooth section. As early as 24 hours after application, scientists observed changes in the shape and structure of pulp cells. Importantly, the team found evidence of potential harm, as restorative materials could reach, damage, and even kill pulp cells by penetrating tiny tubular structures in the tooth section.
Some of these procedures are performed millions of times in one day around the world, and Bertassoni did not expect that the effect on cells would be so noticeable.
In the study, his team found that the use of various restorative materials with biologically active properties promotes the growth of pulp cells and inhibits bacteria that cause caries on the dental chip. Research has demonstrated how the system can help understand the interface of the tooth and gain insight into how dental materials affect dental genetics, health and survival.
Bertassoni suggests the chip could help lead to the development of less harmful dental materials and open the door to personalized dentistry, where doctors could design a chip for each patient to tailor individual treatments.
Danielle Benoit, PhD, from the University of Rochester, and her colleagues, Lisa DeLuise, PhD, and Kathryn Owitt, PhD, are developing salivary gland chips to test drugs that could protect the glands from the side effects of radiation therapy. therapy for head and neck cancer.
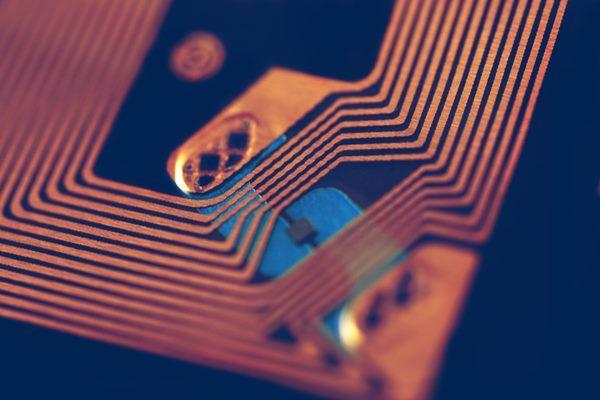
Lisa DeLuise (left), Daniel Benoit (right) and Kathryn Ovitt (not pictured) developed a tissue chip (above) with bubble wells that house tiny cluster-like clusters of salivary glands to identify drugs that protect the salivary glands from radiotherapy for head and neck cancer.

“These chips are valuable as a new tool for studying salivary gland function in vitro,” says Benoit. Their work is supported by NIDCR through the Transnational Institutes of Health's (NIH) “Tissue Chips for Drug Screening” program led by the National Center for Advanced Translational Sciences (NCATS), which aims to develop tissue chips to accelerate the translation of major discoveries into the clinic.
In head and neck cancer patients, radiation therapy can cause permanent damage to the salivary glands, disruption of saliva production, and chronic dry mouth. With enough saliva, people can have difficulty eating and speaking, and are at an increased risk of developing cavities and other oral health problems. A protective drug called amifostine given by clinicians before radiation therapy caused the side effect of a sudden drop in blood pressure. This has led many patients and clinicians to abandon its use.
To find the best radioprotective drugs, the Rochester team developed a tissue chip that contains hundreds of tiny clumps of cells, similar to human salivary glands, for rapid drug screening. Each cluster of salivary gland cells is suspended in a gel-like material and seeded in an aquarium-shaped microbubble that is smaller than a grain of sand. The unique architecture of the vesicles forms clusters resembling globes that make up the actual salivary glands. The tiny environment also concentrates vital proteins and other molecules needed to keep tissues alive and functioning.
In 2021, researchers reported that salivary gland clusters maintain cellular organization, express genes, secrete proteins, and respond to fluid secretion signals in a manner similar to actual salivary glands. They also found that the drug amifostine protected cell clusters from radiation-induced damage, indicating the potential for salivary gland chips to facilitate large-scale drug research. Later, the team plans to screen more than 800 FDA-approved compounds to find radioprotective drugs that could be used to treat head and neck cancer patients.
While the teams at OHSU and the University of Rochester continue to optimize and validate their chips, other NIDCR-supported research is also developing oral-related chips. Some research groups are developing chips that mimic oral barrier tissue to understand gum disease, while others are developing a gum tissue chip to develop treatments for mouth ulcers caused by cancer therapy. Another research group is even creating a “man” on a chip by integrating tissues from multiple body systems; the project is supported by NIDCR and several other NIH institutes through the tissue transplantation program.
“These chips really have the translational potential to open up something that could impact patient care,” says Deluise.
