A gum disease bacteria called Aggregatibacter actinomycetemcomitans may worsen rheumatoid arthritis (RA), according to a study.
Some treatments reduce arthritis symptoms by blocking a person's immune response, suggesting that stopping this pathway could help control RA caused by bacterial infections, the authors write.
“This work highlights how RA may progress through inflammasome activation following bacterial infection associated with periodontitis and discusses the mechanism of inflammasome activation in response to A. actinomycetemcomitans infection,” write the authors, led by Tokuju Okano of the Tokyo Medical and Dental University in Japan.
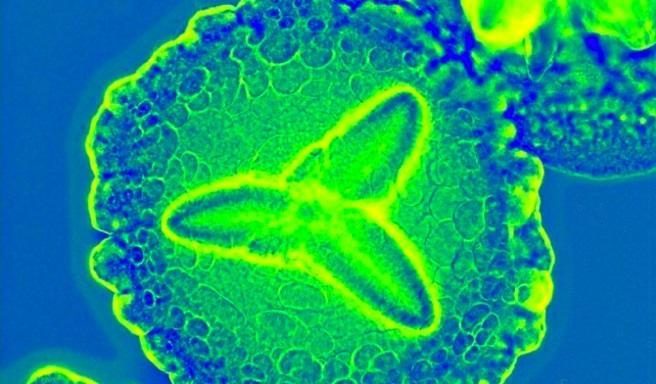
Infection of the peritoneal cavity with A. actinomycetemcomitans worsened RA in animal models by increasing cell activity in the joints and decreasing bone density. This response occurred because the bacteria trigger immune cells to release IL-1β by activating a protein called caspase-11. In a modified mouse model lacking caspase-11, RA and IL-1β production did not occur, highlighting the critical role of caspase-11 in worsening arthritis during infection.
Because the bacteria were not detected in the bloodstream or spleen after oral infection, it is likely that the mouse oral environment prevents the bacteria from spreading. To more accurately model the human disease, the scientists used direct abdominal infection in the study. They found that blocking immune pathways like caspase-11 reduced arthritis symptoms.
Three inhibitors – polymyxin B, chloroquine and an antibody to CD11b – stopped arthritis progression in mice by reducing immune cell activity and IL-1β release in joints. Activation of inflammasomes in immune cells such as macrophages has been shown to play a key role in the exacerbation of arthritis following infection with A. actinomycetemcomitans.
Normally, activation of caspase-11 by bacterial LPS requires a specific transfer process, but LPS from A. actinomycetemcomitans can directly activate inflammasomes. These findings may lead to improved treatments for infection-induced RA or RA with a negative anticitrullinated protein antibody test.
However, because caspase-11 is specific to mice, further studies are needed to understand the role of caspases-4 and -5 in humans, the authors added.
“These findings may pave the way for advances in the clinical treatment of A. actinomycetemcomitans-induced RA or ACPAs-negative RA,” Okano and co-authors concluded.
